In recent years, non-invasive brain stimulation has gained significant attention in both medical and scientific communities. One of the most promising techniques in this field is Transcranial Magnetic Stimulation (TMS). TMS has been celebrated for its ability to treat various neurological and psychiatric conditions without the need for surgery or medications. But what exactly is TMS, and how does it work? Let’s explore the science behind this revolutionary technique and its growing applications in mental health.
What is TMS?
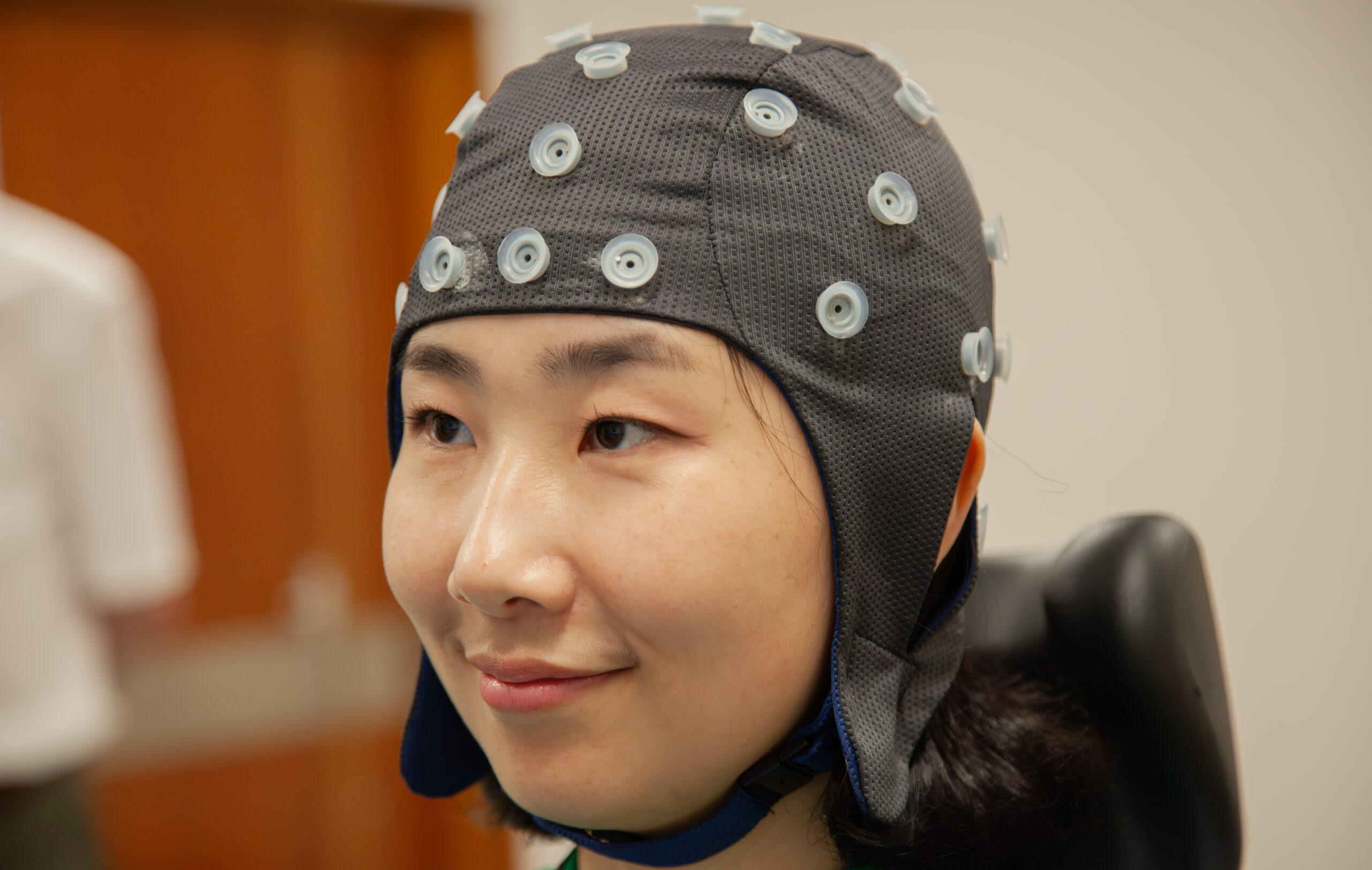
TMS is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in specific regions of the brain. The magnetic pulses, delivered via a device placed on the scalp, are able to pass through the skull and directly influence brain activity. This method of brain modulation is particularly exciting because it allows for targeted stimulation, meaning that specific areas of the brain can be engaged or “reset” to achieve therapeutic effects.
How Does TMS Work?
The procedure involves placing a magnetic coil near the patient’s head. The coil generates short, focused pulses of magnetic energy, which then induce electric currents in the brain. These currents affect neuronal activity, either increasing or decreasing it, depending on the frequency of the pulses. The exact mechanism is complex, but it revolves around the idea that certain mental health conditions—such as depression—are linked to abnormal brain activity patterns. By altering this activity, TMS can restore more typical functioning.
Unlike other brain stimulation methods that require surgical implantation of electrodes, TMS is completely non-invasive, making it a safer, more accessible option for patients.
Applications of TMS
One of the most well-known uses of TMS is in the treatment of major depressive disorder (MDD), particularly for individuals who haven’t responded to traditional therapies like medications or psychotherapy. In these cases, TMS has proven to be an effective alternative, often helping to reduce symptoms where other treatments have failed.
Beyond depression, TMS has shown promise in treating conditions such as:
- Anxiety disorders: Including generalized anxiety disorder (GAD) and post-traumatic stress disorder (PTSD).
- Obsessive-compulsive disorder (OCD): The FDA has approved TMS for treating OCD in certain cases.
- Schizophrenia: While still in the experimental stage, some research suggests TMS may help alleviate symptoms like auditory hallucinations.
- Chronic pain: By targeting areas of the brain involved in pain perception, TMS may offer relief for those with chronic pain conditions.
The Potential Role of VR and TMS
Although not widely integrated yet, virtual reality (VR) could be a powerful complement to TMS therapy. VR-based environments offer immersive, controlled settings where patients can be guided through specific mental or emotional exercises. Combining this with the brain-modulating power of TMS could create tailored therapeutic experiences, enhancing both the effectiveness and engagement of treatments.
For instance, a patient with PTSD could receive TMS while undergoing a VR-guided exposure therapy session, potentially boosting the efficacy of both treatments simultaneously. Research in this area is still emerging, but the potential for personalized, dynamic therapy is intriguing.
Safety and Side Effects
While TMS is generally considered safe, it’s not without some risks. The most common side effects include mild headaches, scalp discomfort, and tingling during the procedure. These are usually temporary and subside shortly after treatment. Rarely, TMS can trigger seizures, though this is exceedingly uncommon when proper safety protocols are followed.
Despite these risks, TMS has a robust safety profile, especially when compared to more invasive procedures like deep brain stimulation (DBS). It also avoids many of the systemic side effects associated with medications, such as weight gain, sexual dysfunction, or digestive issues.
The Future of TMS
As our understanding of brain function deepens, so too does the potential for TMS to expand its therapeutic reach. Current research is exploring how TMS could help treat neurological disorders like Alzheimer’s disease, Parkinson’s disease, and stroke rehabilitation. There’s even interest in its potential to enhance cognitive abilities, though this remains an ethically debated area.
Looking ahead, we can expect to see more personalized TMS protocols. Using advanced neuroimaging techniques, scientists may one day be able to tailor TMS treatments to individual brain patterns, further optimizing outcomes for patients.
Conclusion
Transcranial Magnetic Stimulation represents a significant leap forward in the field of neuromodulation. Its ability to modulate brain activity in a non-invasive, targeted manner has made it a powerful tool in treating mental health disorders, especially for patients who have not responded to conventional therapies. As research continues and new technologies like virtual reality integrate with TMS, we are likely to see even more applications for this cutting-edge therapy in the near future.
For patients and clinicians alike, TMS offers a glimpse into the future of mental health treatment—one where interventions are not only more effective but also safer and more personalized.


 No products in the cart.
No products in the cart.